Laura Ross-Paul gave this speech at the Fuda Hospital International Cancer Forum on July 2, 2016.
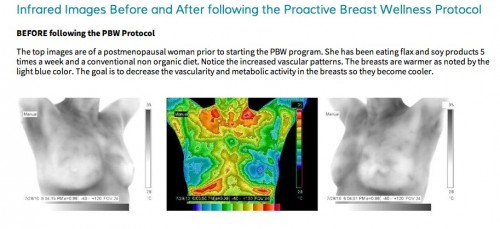
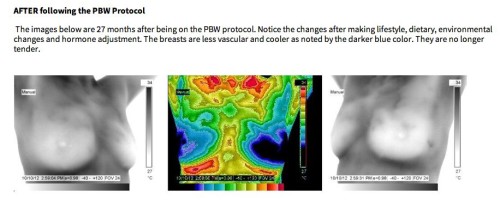
The Early Freeze Protocol is a proposed approach for dealing with “something suspicious” found through early imaging of breast cancer. It is a Proactive cancer preventative measure.




 The Best Breast Cancer Screening Tests
The Best Breast Cancer Screening Tests